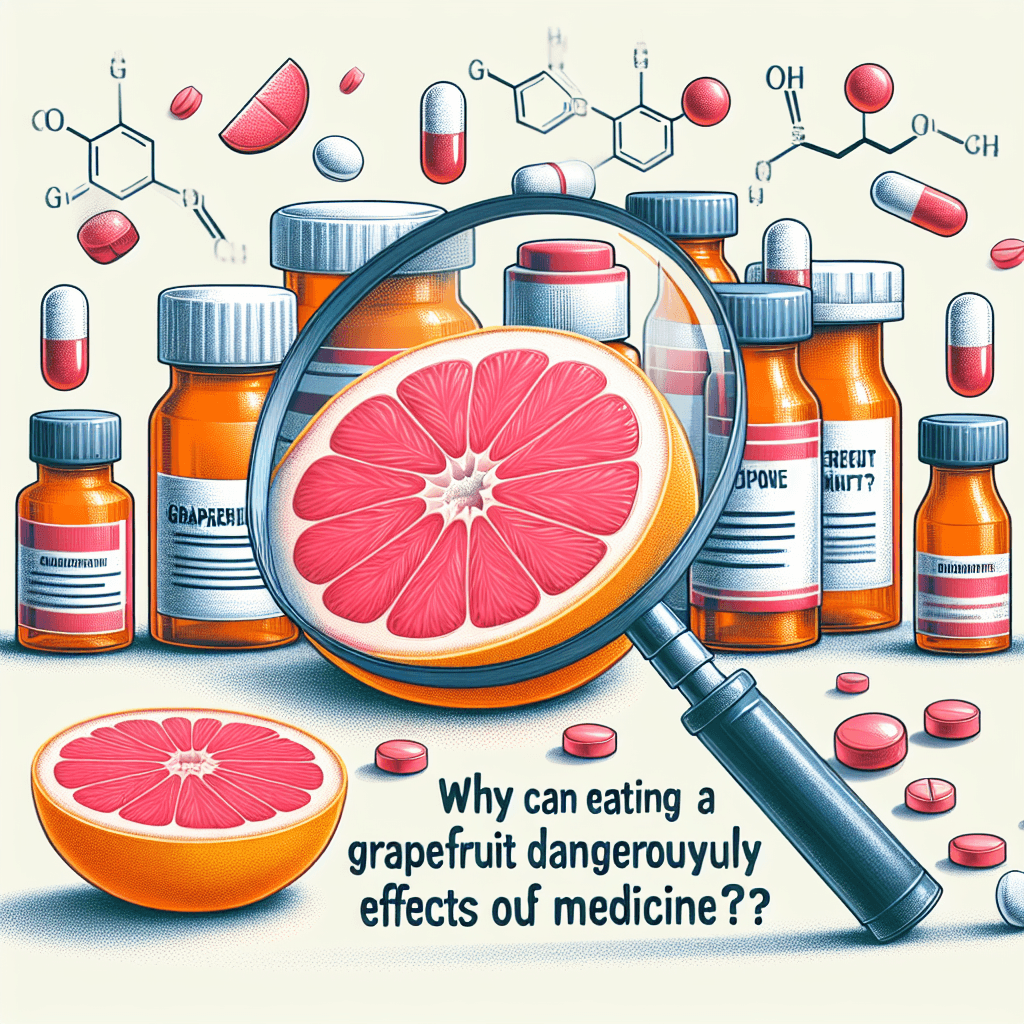
Why can eating a grapefruit dangerously alter the effects of medicine
That healthy grapefruit you had for breakfast could be dangerously supercharging your medication, turning your prescribed dose into a toxic overdose.

Too Long; Didn't Read
TLDR: Grapefruit contains chemicals that block an enzyme your body uses to break down many medications. This can cause dangerously high, and sometimes toxic, levels of the drug to build up in your blood, essentially turning a normal dose into an overdose.
The Bitter Truth: Why Can Eating a Grapefruit Dangerously Alter the Effects of Medicine?
That morning grapefruit, a symbol of a healthy start to the day, could be hiding a dangerous secret. For millions of people on common medications, this citrus fruit can trigger a cascade of unintended and potentially life-threatening side effects. This isn't a health fad myth; it's a well-documented and serious pharmacological phenomenon. This post will break down the science behind why eating a grapefruit can dangerously alter the effects of your medicine, which drugs are most affected, and what you need to know to stay safe.
The Chemical Culprits: Furanocoumarins
The source of the problem isn't the vitamin C or the fiber in grapefruit. The danger lies in a class of natural chemical compounds called furanocoumarins. These compounds are most concentrated in grapefruit but are also found in other citrus fruits like Seville oranges (often used in marmalade), pomelos, and tangelos. While harmless on their own, furanocoumarins have a profound effect on how our bodies process certain medications. They are the key that unlocks this dangerous interaction.
How Grapefruit Hijacks Your System
To understand the interaction, you first need to know about a crucial enzyme in your body called Cytochrome P450 3A4 (CYP3A4). Think of CYP3A4 as your body’s primary drug-metabolizing "clean-up crew." Located mainly in the walls of your small intestine and in your liver, this enzyme is responsible for breaking down a vast number of medications before they enter your bloodstream. This process ensures you get the correct, intended dose.
When you consume grapefruit or its juice, the furanocoumarins get to work. They specifically target and inhibit the CYP3A4 enzyme in your small intestine. The key problem is that this inhibition is irreversible; the furanocoumarins effectively shut down the enzyme until your body can produce more, a process that can take over 24 hours.
This shutdown leads to two main outcomes:
-
Dangerously High Drug Levels: For most affected drugs, CYP3A4 deactivates a portion of the medication as it's absorbed. With the enzyme out of commission, far more of the active drug enters your bloodstream than your body is prepared for. The result is a potential overdose. Taking your prescribed dose with a glass of grapefruit juice can be the equivalent of taking multiple pills at once, leading to toxic effects.
-
Reduced Drug Effectiveness: For a smaller group of medications known as "prodrugs," the opposite happens. These drugs are inactive when you take them and rely on the CYP3A4 enzyme to convert them into their active form. If grapefruit inhibits the enzyme, this activation process is blocked, and the medication may not work at all.
Common Medications Affected by Grapefruit
The list of medications that interact with grapefruit is extensive and continues to grow. According to the U.S. Food and Drug Administration (FDA), many drugs are now required to have a warning label about this interaction. It’s crucial to read your prescription information and talk to a professional, but some of the most common categories include:
- Certain Statins: Drugs for lowering cholesterol, such as atorvastatin (Lipitor) and lovastatin (Mevacor). The interaction can increase the risk of rhabdomyolysis, a serious condition of muscle breakdown.
- Some Blood Pressure Medications: Calcium channel blockers like nifedipine (Procardia) can cause blood pressure to drop to dangerously low levels.
- Organ Transplant Rejection Drugs: Medications like cyclosporine (Neoral) can reach toxic levels, increasing the risk of kidney damage.
- Certain Anti-Anxiety and Antidepressant Drugs: Medications such as buspirone (BuSpar) can have their effects amplified, leading to increased dizziness and drowsiness.
- Some Blood Thinners: Including apixaban (Eliquis) and rivaroxaban (Xarelto), which can have an increased risk of bleeding.
It's important to note that even a single grapefruit or a small glass of juice can be enough to cause a significant interaction. Because the effect can last for up to three days, simply spacing out your medication from your grapefruit consumption does not solve the problem.
Conclusion
The grapefruit-drug interaction is a powerful example of how a natural food can have a significant impact on our body's chemistry. By inhibiting the critical CYP3A4 enzyme, furanocoumarins in grapefruit can turn a therapeutic dose of medicine into a toxic one or render it completely ineffective. This highlights the critical importance of being an informed patient. Always read the labels and information provided with your prescriptions. Most importantly, maintain an open dialogue with your doctor or pharmacist. If you love grapefruit, ask them specifically if it is safe to consume with your current medications. A simple conversation could prevent a serious health crisis.